Programming living cells offers the prospect of harnessing sophisticated biological machinery for transformative applications in energy, agriculture, water remediation and medicine. Inspired by engineering, researchers in the emerging field of synthetic biology have designed a tool box of small genetic components that act as intracellular switches, logic gates, counters and oscillators.
But scientists have found it difficult to wire the components together to form larger circuits that can function as “genetic programs.” One of the biggest obstacles? Dealing with a small number of available wires.
A team of biologists and engineers at UC San Diego has taken a large step toward overcoming this obstacle. Their advance, detailed in a paper which appears in this week’s advance online publication of the journal Nature, describes their development of a rapid and tunable post-translational coupling for genetic circuits. This advance builds on their development of “biopixel” sensor arrays reported in Nature by the same group of scientists two years ago.
The problem the researchers solved arises from the noisy cellular environment that tends to lead to highly variable circuit performance. The components of a cell are intermixed, crowded and constantly bumping into each other. This makes it difficult to reuse parts in different parts of a program, limiting the total number of available parts and wires. These difficulties hindered the creation of genetic programs that can read the cellular environment and react with the execution of a sequence of instructions.
The team’s breakthrough involves a form of “frequency multiplexing” inspired by FM radio.
“This circuit lets us encode multiple independent environmental inputs into a single time series,” said Arthur Prindle, a bioengineering graduate student at UC San Diego and the first author of the study. “Multiple pieces of information are transferred using the same part. It works by using distinct frequencies to transmit different signals on a common channel.”
The key that enabled this breakthrough is the use of frequency, rather than amplitude, to convey information. “Combining two biological signals using amplitude is difficult because measurements of amplitude involve fluorescence and are usually relative. It’s not easy to separate out the contribution of each signal,” said Prindle. “When we use frequency, these relative measurements are made with respect to time, and can be readily extracted by measuring the time between peaks using any one of several analytical methods.”
While their application may be inspired by electronics, the UC San Diego scientists caution in their paper against what they see as increasing “metaphorization” of engineering biology.
“We explicitly make the point that since biology is often too intertwined to engineer in the way we are accustomed in electronics, we must deal directly with bidirectional coupling and quantitatively understand its effects using computational models,” explained Prindle. “It’s important to find the right dose of inspiration from engineering concepts while making sure you aren’t being too reliant on your engineering metaphors.”
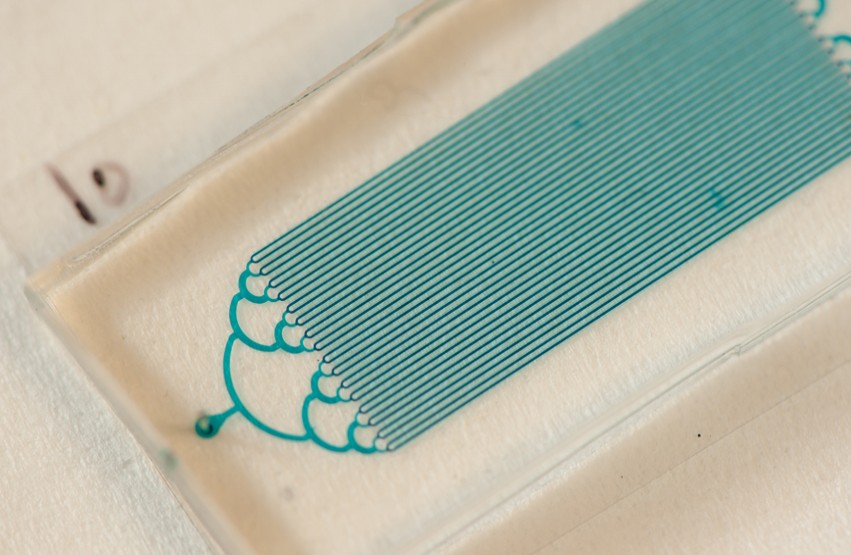
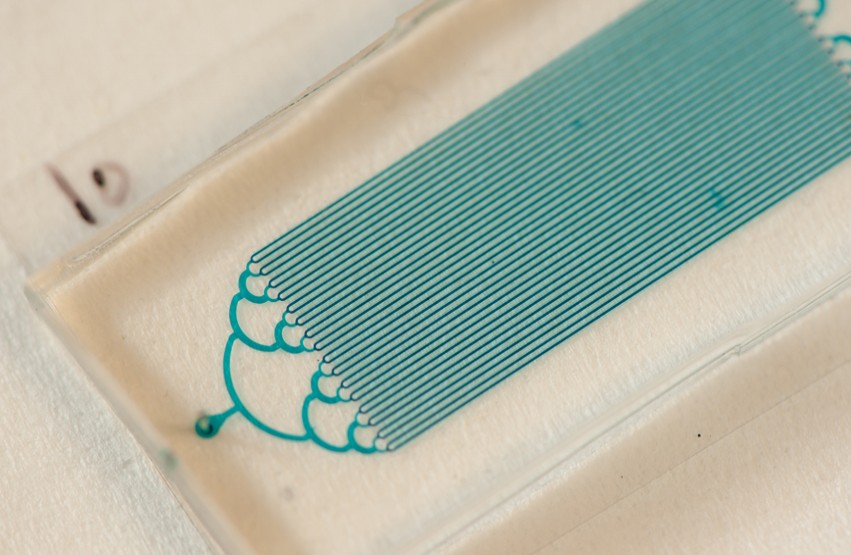
Microfluidic device containing an array of "biopixels" (square traps) in which bacteria grow. Credit: Arthur Prindle, UC San Diego
Enabling this breakthrough is the development of an intracellular wiring mechanism that enables rapid transmission of protein signals between the individual modules. The new wiring mechanism was inspired by a previous study in the lab on the bacterial stress response. It reduces the time lags that develop as a consequence of using proteins to activate or repress genes.
“The new coupling method is capable of reducing the signaling time delay between individual genetic circuits by more than an order of magnitude,” said Jeff Hasty, a professor of biology and bioengineering at UC San Diego who headed the team of researchers and co-directs the university’s BioCircuits Institute. “The state of the art has been about 20 to 40 minutes, but we can now do it in less than one minute.”
“This study is an outstanding example of the power of interdisciplinary systems biology approaches, which treat our cells like integrated pathways and networks instead of a collection of individual components,” said Sarah Dunsmore, a program manager at the National Institute of General Medical Sciences, which finances a National Center for Systems Biology at UC San Diego that supported the research. “By combining the complexity of naturally occurring biological processes with engineering principles, Dr. Hasty and colleagues have produced a model that will provide the basis for creating genetic circuits that can be used to study human health and disease.”
“What’s really exciting about this coupling method is the particular way we did it,” said Prindle. “Rather than trying to build from scratch, we made use of the enzyme machinery that the cell uses for rapid and precise signaling during times of stress. This is an appealing strategy because it lets us take advantage of the advanced machinery that nature has already evolved.”
Hasty credited Prindle for coming up with the idea for the study and carrying it through. “Beyond his modeling and bench skills, I’ve been extremely impressed by Arthur’s ingenuity and drive,” said Hasty. “This project arose from his creativity at the outset and he had the raw energy and excitement to carry it to the end.”
The scientists received funding for their development from the National Science Foundation (MCB-1121748) and by the San Diego Center for Systems Biology (NIH Grant P50 GM085764).
http://ucsdnews.ucsd.edu/pressrelease/uc_san_diego_researchers_develop_bacterial_fm_radio#When:17:00:00Z